Patient Adherence – Special Feature
Still no Rx for patient adherence
Pharma limited in what it can do, but can still have a positive impact
Patient adherence remains a complex puzzle with no simple solutions, and no one stakeholder involved – physicians, insurers, or pharmaceutical companies – can provide all the answers needed. Even though the influence of pharma companies on the patient adherence problem is particularly limited, pharma does have a role to play and there are things the industry can do to encourage better use of medicines, experts say.
The payoff is obvious – better compliance with medications means more sales for pharma. According to CapGemini in a November 2012 report, lack of medication adherence costs the U.S. pharmaceutical industry about $188 billion annually. That amount represented 59 percent of the $320 billion in total U.S. pharmaceutical revenue in 2011 and 37 percent of the $508 billion annual potential total revenue.
“Extrapolated to the global pharmaceutical market, revenue loss is estimated to be $564 billion, or 59 percent of the $956 billion in total global pharmaceutical revenue in 2011, and 37 percent of the $1.52 billion annual potential total revenue,” CapGemini experts noted.
These experts contend that if adherence rates were increased by just 10 percentage points, this would translate into a $41 billion pharmaceutical revenue opportunity in the United States and $124 billion globally, accompanied by improved health outcomes and decreased healthcare spending.
Outside of pharma and in the healthcare arena, one factor pushing the drive for increased medication adherence is the impact of the Affordable Care Act’s Readmission Reduction Program, which started in October 2012. Initially, the program reduced by up to one percent payments to hospitals with excess readmissions for heart failure, heart attack, and pneumonia. This year, maximum reductions increased to three percent of hospital payments and the Centers for Medicare and Medicaid Services expanded the penalty to COPD and total hip arthroplasty (THA) and total knee arthroplasty (TKA).
According to NEHI’s October 2012 brief, “Improving Medication Adherence and Reducing Admissions,” as hospitals improve their discharge planning process and provide transitional care, they are taking into account medication management because more post-discharge adverse events are related to drugs than other causes.
According to NEHI experts, “Researchers have estimated that up to 19 percent of discharged patients experienced an adverse event after discharge, of which roughly two-thirds were attributed to medications. One study found that one-third of adverse drug events resulting in a hospital admission were related to non-adherence. The aggregate cost of hospital admissions related to medication adherence has been estimated to be roughly $100 billion per year and estimates of the share of hospital admissions related to non-adherence are as high a 10 percent.”
What pharma is thinking and doing
Many of the top pharma companies are taking on the issues of medication adherence, but perhaps none so intensively as Pfizer Inc. One section of its website is devoted to papers on the “Value of Medicines,” aimed toward public policy researchers.
According to one of the papers, “The Value of Drug Adherence,” “The CBO estimates that a 1 percent increase in the number of prescriptions filled by beneficiaries would cause Medicare’s spending on medical services to fall by roughly one-fifth of 1 percent.”
Another paper on Pfizer’s site, “The Value of Medicines in Offsetting Healthcare Costs,” also drives home the better adherence equals lower costs message with statements such as, “Improved adherence to diabetes medications could avoid 699,000 emergency room visits and 341,000 hospitalizations annually, for a savings of $4.7 billion dollars. To illustrate these savings, compare the average cost of complications due to uncontrolled diabetes — such as an amputation surgery, which is $40,000, or dialysis for one year for a patient with kidney failure, which is $83,000 — with the average cost of $2,400 for a year’s supply of medicines that help control a patient’s diabetes.”
One of Pfizer’s most visible programs for patient adherence is GetHealthyStayHealthy.com, which was launched during 2013. Topics in the “Managing Your Health” section of the Website give advice on working with a healthcare team; caregiving; tracking your health; evaluating health information; clinical trials; and “Your Medicines: Information and tools to help you take your medicines safely and correctly.”
Within that section are articles about identifying counterfeit medicines, how to travel with medicines, and a video from Dr. Freda Lewis-Hall, Pfizer’s chief medical officer, on avoiding common mistakes in taking medicine.
Another section of Get Healthy Stay Healthy focuses on healthy living topics including “Women’s Health,” “Healthier Aging,” “Vaccines and Prevention,” “Bone & Joint Health,” and “Mental Health.”
The company also has an entire section of its main website devoted to information on patient literacy. “Pfizer has taken a leadership role in promoting clear health communication. We are working with nationally recognized organizations and experts to develop tools and solutions to improve communication between patients and providers.”
Under the “patients” section, besides giving a definition of health literacy, Pfizer tells patients what they can do during a consult: “If the doctor, nurse, or other member of the health care team says something that you do not understand – let them know! It’s their job to explain things clearly. It is important that you are clear about the plan for you or your family before you leave the office or hospital.
“If you don’t understand you can say things like:
• I am sorry, but I did not catch that. Can you say it again?
• I am sorry, but I had a hard time following that. Can you explain it again?
• I am confused about what you said. Can we go over it again?
• I didn’t understand some of the words you used. Can you tell me that again, in less medical terms?”
Pfizer advises health professionals to take “universal precautions” when talking to patients: “This means communicating clearly and in plain language with all patients. This is better than trying to identify and communicate differently with patients who have low health literacy. Since only 12 percent of Americans have proficient health literacy skills, universal precautions are a safe bet.”
The company acknowledges the difficulties physicians have in speaking plainly, due to ingrained habits and education, and also a fear of “dumbing down” the information and insulting patients. “These concerns are not warranted,” Pfizer says. “Patients prefer simple, straightforward communication. Clear health communication helps patients of all levels of education and health literacy learn more about their health.”
Pfizer and other companies are also conducting trials to determine how better medication adherence leads to better outcomes. In February, Pfizer Independent Grants for Learning & Change and Bristol-Myers Squibb Independent Medical Education announced a collaboration to offer a new grant opportunity focused on transitions of care for patients with venous thromboembolism. One of the goals of the grant proposal is “improving patient adherence to prescribed oral anti-coagulation therapy for secondary-VTE risk reduction.”
In September 2014, Janssen Pharmaceuticals Inc. reported the results of a study, “The Impact of JANSSEN CONNECT Injection Centers on Adherence to an Atypical Long-Acting Injectable Antipsychotic among Patients with Schizophrenia Enrolled in a Support Program.”
The title is less than snappy, but the results are worth taking note. According to Janssen, the study showed that Janssen Connect patients who received their Janssen long-acting treatment (JLAT) at an injection center – typically a pharmacy – and remained in the program for more than six months were 4.5 times more likely to be adherent to their medication than those within the program who did not select this offering.
“The Janssen Connect program was born out of our dedication to helping people living with schizophrenia navigate through the difficulties of living with the disease and staying on medication as prescribed by their healthcare provider,” says Catherine Tak Piech, VP, Health Economics and Outcomes Research, Janssen Scientific Affairs LLC. “People living with schizophrenia can live productive and meaningful lives, and these results are proof that we’re moving in the right direction to help them do just that.”
For people living with schizophrenia, non-adherence to antipsychotic medication is high. A study published in the June 2014 edition of the journal Patient Related Outcome Measures estimates that up to one-third of all schizophrenia patients are not taking their medicines as they should. Patients who are non-adherent are at increased risk of relapse and hospitalization, possibly leading to disability, homelessness, incarceration and other serious consequences. Janssen says about 80 percent of patients with schizophrenia who responded to treatment of their first episode experience a relapse within five years.
The Janssen study further showed that 87 percent of patients enrolled in Janssen Connect who received their medication through the program achieved medication adherence.
Through Janssen Connect, patients can find injection centers, often pharmacies, where patients can receive their injected long-acting medicines at a more convenient location than a physician’s office. In addition to having the option of receiving their treatment at one of these locations, patients receive reminder alerts the day before their appointments. Their visits are documented, and their physicians are notified if they miss their injection appointments.
“While the effect of locations for long-acting injections on reduction of barriers to health care professional-ordered injections is unknown, this study helps support the option that the injection center locations may be helpful to patients,” Janssen executives say.
Back in 2012, Janssen launched CareForToday, a secure messaging platform, mobile application and website (www.care4today.com). The mobile platform is designed to improve adherence to treatment regimens through reminders to take medications, refill prescriptions, and visit healthcare providers.
“Janssen Healthcare Innovation is developing products and services to transform the patient experience and promote better health outcomes. We have identified improving medication adherence as one of our key initiatives,” says Diego Miralles, M.D., head,
Janssen Healthcare Innovation. “The Care4Today Mobile Adherence platform can help overcome the number one barrier to consumers taking their medications by providing customized reminders delivered via secure messaging directly to their cell phone, a device that most people carry with them at all times.”
What else can pharma do?
Advertising and marketing experts who work with their pharma clients say before a program can be put together to address patient adherence, the factors of nonadherence should be determined.
Simon Smith, VP of strategy for Klick Health, says the main barriers to adherence are efficacy, safety, and cost.
Efficacy is often less about the actual efficacy of the drug and more about how a patient perceives how effective it is, Smith says.
“The first thing in the patient’s mind is am I feeling better or is it addressing the symptoms,” he says. “Oftentimes, that might not happen for two to four weeks, and if the expectation isn’t set properly, they’re not going to see the results and they are going to be less inclined to continue with that behavior.”
This is why it’s particularly important that pharma is careful to set expectations with its products, making sure patients understand when the product is going to be working and what is the common period of time it would take for them to notice that, Smith says.
The flip side of efficacy as an adherence barrier are side effects. “Side effects are a big barrier to patients, especially if they are not seeing efficacy,” Smith says. “Sometimes they feel the side effects before they feel the effect.”
Smith has observed that with many of Klick’s pharma clients, their first inclination is to downplay side effects. “They might have the ISI on a Website but they’re not going to create content around side effects,” he says.
Conversely, he sees that patients have a great curiosity about side effects and want to find out as much information as possible.
“What we see from data, like search data, if [patients are] considering the product, if they’re on the product, actually they’re researching side effects on a pretty regular basis,” Smith says. “They might type in a drug name followed by ‘side effects’ to understand side effects they might have or side effects that they have currently.”
Pharma is missing an opportunity to connect with patients by not offering information, Smith told Med Ad News.
“If we don’t have content on our website that’s directly addressing the side effects patients are experiencing or worried about experiencing, they’ll go somewhere else to learn about them, and we won’t have the opportunity to train them and talk to them about how they might be able to mitigate them,” Smith says.
Klick advises their clients to be transparent about side effects and set expectations, Smith says.
The third big adherence barrier is cost. Most pharma companies are addressing that barrier by providing discount cards and similar programs.
“It’s become fairly standard, I think 75 to 85 percent of the brands I work on use a savings card,” Smith says. “And those that don’t, it may simply be that the product may be a biologic or they have some other way to deal with the financial part of it.”
According to Smith, savings cards are a “hard” tactic, as opposed to soft, in the sense that a card is a tangible thing that gives patients dollars off their prescriptions.
In addition to actual discounts, cards provide a value proposition. “I think we forget that patients are consumers,” Smith says. “If they’re taking a pharmaceutical product for a chronic illness and there are other options for them for treating it, we often don’t think about the full consideration of that. We’re often thinking of, ‘my product versus a generic,’ or ‘my product versus another branded product.’
“In reality, from a patient’s perspective, there may be over-the-counter treatments, there might be dietary solutions that they can implement, there may be other ways for them to potentially achieve the same impact. So we really need to talk to them about the value proposition.”
A patient may be paying a $50 or $75 co-pay for a drug, but might have to spend far more than that if trying to deal with their condition using an over-the-counter product they will have to pay out of pocket for, as well as additional time and effort.
And if a payer is not covering a product, the main reason is economic outcomes, and the payer will need convincing as well, Smith says. “Yes, there’s a cost here to the patient and a cost here to the payer, but the alternative to not treating or undertreating or treating with an over-the-counter product or trying to use some dietary intervention is going to potentially have longer-term health implications in cost – and also cost more in the short term,” he says.
Irritable bowel disease is one example of where patients can pay more in the short term for an OTC product while experiencing longer-term health implications that will cost more in the long term, Smith says. “Laxatives are what comes to mind, those can be expensive over the long run, and the co-pay might actually be cheaper,” Smith says.
The key to designing a better adherence program is making it relevant to the disease state, says Kim Radefeld Sr., director of healthcare solutions at C3i Healthcare Connections.
“Is it a chronic disease, like diabetes, or is it an imminently life-threatening disease, like some level of advanced cancer?” Radefeld says. “It makes a big difference in how you design your programs.”
The complexity of the therapy also has to be considered, she adds. “Is it a pill you’re asking the patient to take on a regular basis, or is it four or five hours out of their day to go to an infusion center? These are very sophisticated medications with very serious side effects.”
For therapies that are just a pill, easier ways to make sure those patients are filling their prescriptions and taking their medicines could be a co-pay card and some tech-based reminders. “On the other hand, is it a very complex therapy for a very critical disease in an acute phase? Then you need to reach out and create a very robust patient engagement program that has healthcare professionals working with those patients to overcome very specific adherence barriers that they will encounter,” Radefeld comments.
Adherence barriers could even be individual to each patient, Radefeld added.
“Personally, I’m very adherent on some things and very nonadherent on others,” she says. “It would be incumbent on a nurse or other healthcare professional to figure out why am I adherent to some of the things I’m told to do by my physician, but not adherent to everything.”
For example, a patient with diabetes may be experiencing barriers of knowledge, cost, and silent symptoms. A patient may think only older people get diabetes or understand that “high sugar” is a symptom; not knowing whether insurance will cover the cost of a treatment or how much they will have to pay; or they just feel generally fine and will not believe they have diabetes.
Fear of side effects may also come to play, Radefeld says: “‘My doctor wants me to take this new drug, but I heard from my neighbor that it could hurt my liver,’ so that could put a barrier there of who do you listen to? Who is relevant to that patient as far as their adherence program? Is it what their doctor tells them or is it what their neighbor tells them? And different patients react in different manners.”
Radefeld also pointed to a “multidimensional adherence obstacle,” in that patients do not have the social support necessary to do what they know they should be doing. “The example I give here is, ‘My husband told me I was silly to listen to that nurse, he’s not going to remind me about doing blood testing because he doesn’t think I have the disease and I’m just uncomfortable testing my blood myself,’” Radefeld says.
According to Radefeld, to address the barriers to adherence, companies need to create messaging and channels and usage that is relevant, making sure that the message is conversational and engaging and does not add to patients’ issues.
“The company should provide clear information on its patient engagement or adherence program, clear information about the therapy they’re talking about to patients, and the resources patients might have available to them,” she says. “It’s all about communicating, and communicating to the patient in a manner that they’re going to respond to.”
The messages should be disseminated in an environment or multichannel environment. “Some patients are going to respond well to that phone call, and some say ‘I would love a text message, just to remind me to do something,’” Radefeld told Med Ad News. “Others like e-mail, some patients like online community groups. It’s a whole array of how to talk to a patient via a channel that they want in a manner that’s appropriate to them.”
And each time a company interacts with a patient or consumer, it should be tracking when and how the interaction happened, and perhaps track the results of the interaction, if possible. “Every interaction with the patient needs to be assessed and tracked, so you can take that into the aggregate reporting and related analytics,” Radefeld says. “Based on that tracking and aggregate reporting and analytics, you can determine how effective your program is, and you can determine what in your program is really working well for you and what can you modify or optimize to improve the effectiveness of your program.”
The data will tell the truth, even when a company wants to believe otherwise.
“We’ve found out more than once, messaging that we thought would really be effective and we’d worked very diligently on with that advertising agency, sometimes it doesn’t work, even with our best efforts,” Radefeld says. “If you’re assessing those reactions, you’re going to find out pretty quick that that’s not working. [The message] may be too convoluted, or in pharma’s case, the lawyers got hold of it and now you need to do something about it. But you can identify those areas of opportunity, to take the assessment information, and not only would you know the nuts and bolts of what’s working within your company, you’ll be able to quantify how you’re moving the dial on it.”
Health literacy and gamification
One area of adherence where pharma companies can have a big impact — as Pfizer has been advocating — is in health literacy.
“We know that health literacy affects adherence,” says Christine Mullen, director of health strategy and innovation at Cadient. “There’s variation on how directly and how many numbers and how much dollars and all of that, but what we do know is that it definitely affects it, one way or another.”
According to Mullen, there are three specific tactics the Department of Health and Human Services recommends for tackling health literacy problems. One is the “teach back” technique, in which the healthcare practitioner, after explaining to the patient what their treatment options are, asks the patient to say everything back to the HCP.
“People don’t understand basic things. You and I, we understand what ‘injection’ and ‘oral’ means, but the typical American actually gets tripped up on that,” Mullen told Med Ad News. “I’ve heard little anecdotes about a woman with a child with an ear infection who actually, because it was a syringe-based medication, was putting the medicine in the child’s ears, instead of giving it to them by mouth, because the directions weren’t clear enough.”
A second tactic, and one pharma can definitely employ, is putting together non-language dependent materials, which use pictographs, images or photos.
The third recommended tactic, which is usually employed by the pharmacy, is personalized health sheets that can keep track of which patient is taking what kind of medication and be used to generate very specified and customized kind of communication.
According to Mullen, digital campaigns and tactics, like those created by Cadient, offer clients ways to act on these recommendations. “Digital is perfectly aligned to get those things, there’s a lot of opportunity within each of those three pathways of recommendations to start making some impact there,” she says.
Digital is the only medium that can touch all seven ways that people learn: linguistic, logical, spatial, musical, audible, genetic, and interpersonal/intrapersonal, Mullen says.
“People learn either socially or on their own,” she says. “They like to hear things, they like to see things. So what we try to do is, when people are coming to your digital experience, your Website or digital tool, it’s going to cross the gamut of literacy. There are people who are going to be very low functional or very high functional. So what you want to do is try to offer as many different ways people can learn about your product or about your service. And the way you can do that is by utilizing your whole digital platform around the seven ways of learning.”
Patients in certain therapeutic categories have more of a struggle with health literacy than in others, Mullen notes.
“People who are challenged more with health literacy are the older population, typically 65-plus,” she says. “We also know 65-plus has the largest amount of chronic illness. Ninety-nine percent of Medicare spending is based around chronic disease. Those two numbers are pretty aligned to each other. The other population base that deals a lot with chronic illness is the lower income, a lot of minorities, especially diabetes and cholesterol, things that are very lifestyle-oriented.
“But you even see it in things like cardiovascular where you have people with a lot of comorbidities, and again, this goes back to the whole 55-plus age range – when we start to add in more pills, more treatments, more things you have to do, human nature is that they start to grapple with what they are understanding, keeping it all together and what they’re taking when.”
Where there is less of a health literacy problem is disease states where people have a very tightly entrenched caregiver relationship, conditions such as Parkinson’s disease or cancer. “You’ve got a spouse, a child, a friend, a neighbor, or whoever, but you also have a very full, professional care team,” Mullen says. “Health literacy becomes less of an issue with Parkinson’s because you have somebody who’s living this in their daily life, they’re really entrenched in it and they’re very educated about what’s happening to their bodies. They’ve had it awhile, they have a lot of support around them.
“And a cancer patient, particularly someone who is in relapse, they’re much more educated about what’s happening to their body, in addition to constantly looking for new research because they’re at a critical stage where they don’t want to go back into relapse. When you’re in a more significant life-affecting situation, people are much more health literate in those environments.”
One of the more popular discussions about adherence trends is the use of gamification to enhance the effectiveness of programs. HealthPrize is the most-well-known of gamification in healthcare companies, and has been working with some of the top pharmaceutical companies. HealthPrize has issued case studies in the acne and the injectable diabetes medication areas, in which patients receive points they can use to “buy” rewards such as iTunes gift cards.
But other than what HealthPrize is doing, Smith has not seen a lot of implementation of gamification in the pharma arena. “There are a couple of reasons for that: one is that the concept, even the word, sounds like something people don’t want to mix with medicine, so there’s often that resistance,” he says. “Often people will say, ‘Gamification? This is a serious medical disorder!’”
Once that obstacle is overcome and clients are shown the programs that are working, a new level of discomfort arises because of the incentives. “One is can we really incent patients to pay or take their medication, and if we do that, we have to fund those payments,” Smith says. “So you pass though two levels of discomfort, one to get people over the idea of it and understand why it can be valuable, and then there’s the actual implementation of it. Once they understand that incentive-based programs tend to perform best, now they become uncomfortable about actually incentivizing a patient to take their medication. So we tend to get a lot of interest, because it’s sexy and something a lot of people are talking about, but not a lot of actual implementation.”
Still, there can be a place for gamification in pharma and healthcare, Mullen says. “Gaming can help you learn in a couple of different ways,” she says. “One is in that kind of question and answer quizzing game, where you’re going for that teach-back theory where you learn something and are forced to think about it again, and answer that question again. The other side of it is that more immersive experience, for the more visual learners. That’s someone who is for example, trying to explain what a hallucination means for somebody learning about psychosis. How do you determine the difference between delusions and hallucinations, because for a layperson it’s probably all the same thing? Actually it isn’t, there’s nuance there. So how can you create an actual immersive experience that can teach someone … and that’s where the gamification and education bridge starts to come together and become really cool.”
======================
Physicians to pharma: Co-pays are best
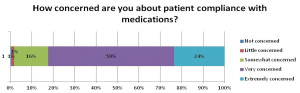
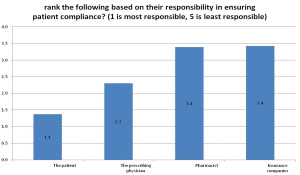
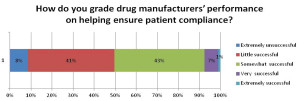
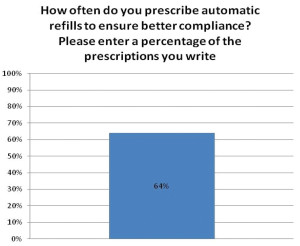
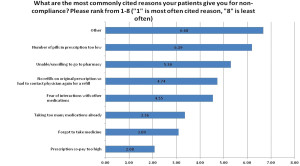
Med Ad News asked Healthcasts to survey its physician base to determine their attitudes toward patient adherence and how pharma could help. Surveying 119 healthcare practitioners, Healthcasts found that 83 percent of physicians are very/extremely concerned with patient adherence; and though most drug manufacturers put substantial effort into ensuring patient compliance, about 49 percent of HCPs feel they have been unsuccessful in those attempts.
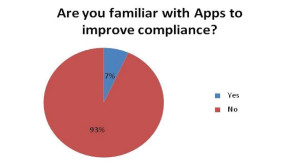
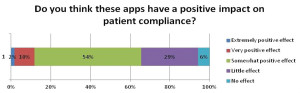
Only 7 percent of physicians said they are aware of apps that could increase compliance, and 35% feel that these apps have a small effect or no effect on patient compliance.