Developing value-added strategies for today’s empowered patient
By Amy Parke, senior VP, Ashfield Healthcare Communications Co.
A new dynamic has evolved over the past decade within the healthcare delivery marketplace. No longer do patients sit meekly and blindly follow direction. Today’s patients are more likely to arrive at their appointment informed about their disease, ready to engage with their physician and take an active role in the treatment and tracking of their condition. Indeed, according to a study published by the Pew Research Center, 72 percent of people using the Internet indicated that they looked online for health information in 2012 and 70 percent of U.S. adults say they track at least one health indicator. Physicians, on the other hand, overburdened and pressed for time and outcomes-based disease management, are looking to the pharmaceutical industry to provide the resources, direction and education patients need to best manage and/or improve their condition.
Addressing this dilemma is a significant challenge to the industry. Faced with these empowered patients and overburdened physicians, the industry can no longer mandate treatment but must find ways to bridge existing gaps between itself and the physicians and patients it serves. True collaboration between all parties will be needed to ultimately change the conversation to deliver the value added strategies that patients want and need to better understand, track and manage their disease.
Creating the patient journey map
In order to foster a collaborative spirit between all parties, the industry needs to pursue a holistic approach to treatment and use this approach as a basis for how it communicates to both patient and physician. Disease impacts far more than the body and the patient alone. From diagnosis to cure or end of life, the patient follows a really long road – one with bumps and deviations; one changed by learning style, by income, by family dynamic. It’s hard, personal stuff and must be treated as such.
In order to respond appropriately with meaningful tools and conversation, pharma needs to capture data on both the emotional and physical impacts of the disease all along the patient’s journey. Aspects such as medical routines, diet and exercise regimens, work and lifestyle customs, key relationships, as well as impact on the patient’s self worth should be carefully monitored and analyzed. From this data, one can create a patient journey map that distills insights into a concise, visually compelling story. Such maps highlight the different stages that patients will go through from before taking action to finally managing their disease. As such, patient journey maps help to identify relevant channels and meaningful content for each stage that will provide the patient with the proper support throughout the journey.
For example, patients diagnosed with a chronic condition such as diabetes might go through five major phases in the disease journey, including:
1. A recognition of initial symptoms fraught with denial, lack of understanding and possible impact on social status. In this phase they are seeking information and reassurance and may turn to self-diagnosis sites, their friends and families, news outlets, and patient online forums.
2. A diagnosis and treatment influence phase, again where there is denial and a lack of understanding with ramped up peer pressure and indecisiveness on the best course of action. Here patients are working with their physician, information websites and possibly their employer or insurance company on possible treatment options.
3. A decision making phase where they are working with their physician and the physician’s office staff as well as websites to better understand their treatment and its side effects as well as the lifestyle changes they may need to make. Patients might be addressing needle phobia or how to get educated at home.
4. An Initiation phase where treatment begins perhaps reluctantly, and the patient deals with lack of nurse follow up or at-home education. Questions arise on disease progression and peers’ advice and online support is often sought.
5. An adherence and management phase where those using injectables often face fatigue and adherence drops off. Mobile apps for tracking may be employed and the patient looks for emotional support from caregivers, friends and patient advice forums.
The right content in the right place
Understanding the steps and emotions patients go through in dealing with their diagnosis and treatment helps to frame the discussion and lead to the development of much more valuable content addressing patient concerns at each step. Once created, it should be curated (filtered, aggregated and collated in a meaningful way) and then syndicated throughout the various channels to offer exposure wherever patients and their caregivers might turn for education and support.
However, creating the right content to disseminate, content that is engaging and understandable, can be a challenge. Indeed, the pharmaceutical industry has a long history of creating ads that look like contracts, websites that look like ads, social media interfaces that are actually anti-social and using language that generally needs a physician to interpret. Although much content creation has been developed to address the regulatory environment in which we operate, we can do much to make our content more readily understandable. To do so, we need to embrace basic learning principles such as those in the following checklist, and properly address the health literacy of our audience throughout their journey.
Checklist for improving the usability of health information
• Identify the intended users
• Use pre- and post tests
• Limit the number of messages
• Use plain language
• Practice respect
• Focus on behavior
• Check for understanding
• Supplement with pictures
• Use a medically trained interpreter or translator
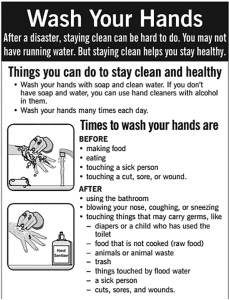
A case in point is the flyer shown below, developed by the Centers for Disease Control and Prevention. Not only does the flyer employ simple language and use graphics to illustrate the main points, it was developed in multiple languages to support all demographic groups in the United States.
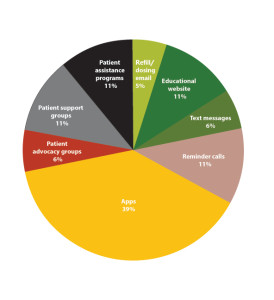
Equally important to creating the correct content is connecting to people where they would most likely seek information. This can range from brochures in their physician’s office to brand and disease websites and social media platforms. Each channel will require its own content, tailored to engage the patient within that channel environment. Figure 1 demonstrates the patient outreach activities most likely to increase through 2017 according to a Cutting Edge report issued in 2012 – a combination of personal and digital contacts with a heavy emphasis on apps.
As the U.S population matures and current baby boomers are replaced, outreach activities will incorporate more social media and texting, requiring a shorter, more conversational communication dynamic to engage the patient.
Harnessing technology to make patients’ lives easier
As shown in the chart below, the race to embrace technology to improve healthcare is on. Informative websites, social media platforms, the use of apps on smartphones, notebooks and electronic devices such as FitBit and the AppleWatch are creating new options for reaching patients to help them monitor and/or manage their disease. These are truly offering platforms for the delivery of value added strategies, some even offering healthy recommendations. Certainly Cutting Edge’s prediction of apps constituting 39 percent of patient outreach by 2017 is telling. Use of the Internet by patients and their caregivers is also growing with the spread of broadband.
Patients suffering with chronic diseases are turning to such Internet tools as the support groups of MendedHearts and DailyStrength, and message boards and forums such as CancerCompass and HealthTap or games such as Fitocracy and Diabesties. Wearable biometric tools and digital health trackers are replacing subjective patient diaries, resulting in the collection of objective data the physician or care provider can use to better assist patients in managing their disease. Consider Sanofi’s blood glucose monitor or Withing’s blood pressure cuff. These are designed with simple, consumer interfaces and plug easily into our favorites devices for self tracking. Some can even send data to the physician’s electronic medical records system. Although pharma cannot access that information due to patient privacy laws, data companies are working to integrate providers with the pharmaceutical industry to deliver key data in the not too distant future. Such integration should only help to improve our overall healthcare delivery system.
It’s an exciting frontier we face but one where we can best serve patients by tapping technology to deliver engaging interfaces that foster adherence or deliver easily absorbed and understood content along their journey. Consider DIDGET. A parent developed this type 1 diabetes monitoring tool for Bayer to create a first-of-its kind glucose meter that connected directly to a Nintendo game system. Now the son who was constantly losing his glucose monitor, but could always find his Game Boy, was able to manage his diabetes with a gaming system that rewarded his good habits.
This is just one example of the right content delivered to the right place, harnessing the power of technology to make the patient’s life easier. By persisting in the development of engaging content delivery strategies and disease management tools that map to our findings in the patient journey, we are truly providing the patient with value added strategies to help navigate their disease.
===========================
Meeting the challenge of physician and patient collaboration along the journey
In order to successfully impact outcomes, physicians must collaborate with their patient along the disease journey. Just as the patient needs support from multiple sources along the way, so does the physician. Although physicians have been quick to adopt technology, outpacing the general population in smartphone adoption for example, they are slow to incorporate new technologies such as FitBit into the patient’s overall care plan. To address this, pharma needs to bring the same journey mapping approach to how they interact with physicians. Just like the patient, the physician travels a path in understanding and treating a disease. The figure below illustrates a hypothetical physician journey which could encompass phases such as awareness, realization, consideration, action and acceptance – where in each phase the physician turns to different channels to obtain content. By making it easy – delivering appropriate educational content and support in each channel where and when the physician needs it – pharma will better equip the physician to collaborate with patients along their journey.