Top 3 Pandemic-Related Health IT Technologies and What to Expect
Top 3 Pandemic-Related Health IT Technologies and What to Expect
By Inga Shugalo
As the pandemic wreaked havoc across the United States, healthcare providers started deploying various health IT solutions to address emerging challenges. They aimed to reduce the load on doctors and protect clinicians and patients from the virus exposure. This approach helped providers continue to deliver due care and avoid closure. According to a report published by the American Healthcare Association (AHA), shut-downs became a painful reality for about 8% of the respondents, which is equal to 16,000 private practices nationwide. Moreover, more than 75 percent of them were specialists. So, what are those life-saving technologies that allowed providers to stay afloat?
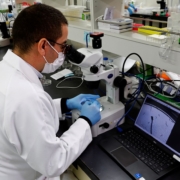
Medical image analysis
During the acute phase of the pandemic, healthcare image analysis became a key assistant in diagnosing coronavirus-related pneumonia. Well-trained deep learning models helped practitioners save time by performing analysis sometimes 10 times faster than human experts. Moreover, AI-driven tools of this kind have shown higher diagnostic accuracy, in some cases.
For example, a medical image analysis solution developed at the University of Wuhan outperformed professional radiologists. Chinese specialists created an ML-driven system analyzing patients’ data (age, gender, and more) and CT scans. When the researchers compared the system’s performance with that of radiologists, they found that the tool detected a COVID-19 infection in 68% of patients whose CT medical experts considered normal. Hence, deep learning models can find complex patterns the human eye can’t perceive.
Deep learning models can also analyze chest X-ray scans successfully. Though the accuracy of such tools is up to 86 percent, with adequate training, they can reach that of the CT scans analysis accuracy. Given that an X-ray scanner offers higher portability and lower cost, the current level of accuracy is acceptable. Such ML-based solutions may help clinicians diagnose the disease earlier, administer treatment on time, and avoid comorbidities.
What’s next?
COVID-19 diagnostics is not the only field of medical image analysis application. AI-driven analysis can assist doctors with pulmonary function testing (PFT) for COPD diagnostics and risk prognostication, diabetic retinopathy and tuberculosis detection, diverse cancer-types diagnostics, including melanoma, breast and prostate cancer, and more. In addition, image analysis is not only for CT or X-ray scans. Adequately trained deep learning models can read ultrasound, microscopy, endoscopy and other types of medical images.
Telemedicine
Deploying telemedicine solutions allowed providers to continue offering remote consultations. Patients have picked up the idea enthusiastically—in one year, the share of telemedicine consultations tripled, from 20 percent in March 2020 to 60 percent in March 2021.
To help doctors with telemedicine tech adoption, specialists from the Stanford School of Medicine prepared a guide. It concisely describes five steps a typical televisit contains, from preparations doctors need to take before each consultation to monitoring a patient’s home environment and their emotional state. Besides, the federal government took the necessary measures to motivate doctors to use telemedicine tools by introducing regulations ruling that teleconsultations and regular in-house visits should be reimbursed equally.
What’s next?
As the situation with COVID-19 has improved, the number of telemedicine visits has been reduced. However, the new care provision model has gained a strong foothold in providers’ services. It has become a good alternative to some in-house therapies.
Telemedicine has proved efficient for managing some behavioral issues (such as anxiety and depression). It allows providing physiotherapy for diverse musculoskeletal conditions, pain management and injury rehabilitation. Telemedicine has also become a standard offer for some nursing homes, sparing immobilized residents the need to go to offline consultations.
Remote patient monitoring
During the pandemic, caring for patients with chronic conditions increased in complexity. Fortunately, providers have had an ally at their disposal—remote patient monitoring (RPM) technologies. RPM devices are numerous: blood pressure monitors, pulse oximeters, blood glucose monitors, spirometers, and more. Using such devices, patients can continuously collect their health data and send information securely to their providers. In the event that a parameter drops or rises to a critical level, the tool notifies the doctor, the patient’s relatives, and the emergency care unit. This care model has allowed patients and providers to reduce human contact to a minimum, thus lowering potential virus exposure.
What’s next
While popular with some share of chronic-condition patients, RPM devices haven’t met the expectation of others. The reasons vary—some patients have difficulty managing the device, others can’t enjoy the solutions due to their cost or connectivity disruptions.
Though efficient for prevention, RPM programs providers offer require regular payments. This discourages many patients who may enroll in such a program once but are unlikely to continue the enrollment for another year.
As we remember, RPM devices can improve the access to care for patients living in remote or rural areas, sparing them the need to travel to their provider’s location oftentimes. However, the efficient work of such devices requires broadband coverage. Otherwise, providers won’t receive a patient’s health data on time and won’t manage to intervene to solve the health crisis.
To provide care for those left behind, providers have started offering device-free patient monitoring. Doctor-patient communication in this case goes over a mobile device or landline phone. Every week, medical professionals prepare questionnaires to evaluate a patient’s health status. When a patient fills in the questionnaire, their doctor calls them to explain the results and consult on further actions.
Today behavioral health makes the most popular choice for device-free patient monitoring. However, Esse Health, a provider-patient community, has leveraged this model for heart failure, COPD, and patients with diabetes, too.
Summing up
Automated image analysis, telemedicine, and RPM have helped providers deliver care effectively amidst the pandemic crisis. These solutions have allowed them to reduce workload and keep some patients safely at home, thus lowering the risk of exposure for both parties.
Providers continue to adapt to the new care models to patients’ needs. We see an increasing number of fields in which image analysis and telemedicine can be used, and a new way to provide patient monitoring to improve access to care for patients from remote and rural locations. Given providers’ flexible approach and attention to patients, we can safely conclude the solutions are here to stay. And with time, they will only evolve.
 |
Inga Shugalo is a healthcare industry analyst at Itransition, a custom software development company headquartered in Denver, Colorado. She focuses on healthcare IT, highlighting the industry challenges and technology solutions that tackle them. Shugalo’s articles explore diagnostic potential of healthcare IoT, opportunities of precision medicine, and robotics and VR in healthcare. |